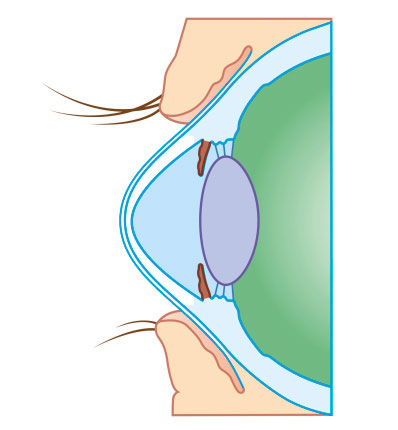
Keratoconus- Corneal Bulge
The information below has been provided with permission from the National Keratoconus Foundation (NKCF).
What Is Keratoconus?
(Ker-a-to-co-nus)
Keratoconus, often abbreviated to “KC”, is a non-inflammatory eye condition in which the normally round dome-shaped cornea progressively thins causing a cone-like bulge to develop. This results in significant visual impairment. Keratoconus may cause substantial vision distortion, with multiple images, streaking, and extreme light sensitivity. The early symptoms of the disease may look no differently than normal refractive defects of the eye. It is important to know more about keratoconus, because it often times goes undiagnosed, and has to be confirmed with corneal topography.
Who Gets Keratoconus?
The actual incidence of KC is not known. It is not a common eye disease, but it is by no means rare. The prevalence for keratoconus in patients range from 1 in 500 to 1 out of every 2,000 persons in the general population. Keratoconus is generally first diagnosed in young people at puberty or in their late teens. It is found in all parts of the United States and the rest of the world. The disease is observed more frequently in certain ethnic groups, like South Asians, or associated with certain diseases, like Down Syndrome.

What Happens? Corneal Bulging.
The cornea is the clear window of the eye and is responsible for refracting most of the light coming into the eye. Therefore, abnormalities of the cornea severely affect the way we see the world making simple tasks, like driving, watching TV or reading a book difficult. In its earliest stages, keratoconus causes slight blurring and distortion of vision and increased sensitivity to light. These symptoms usually first appear in the late teens and early twenties. Keratoconus may progress for 10-20 years and then slow or stabilize. Each eye may be affected differently.
What Can Be Done About It?
In the early stages, eyeglasses or soft contact lenses may be used to correct the mild nearsightedness and astigmatism caused in the early stages of keratoconus. As the disorder progresses and the cornea continues to thin and change shape, rigid gas permeable (RGP) contact lenses are generally prescribed to correct vision more adequately. The contact lenses must be carefully fitted and frequent checkups and lens changes may be needed to achieve and maintain good vision. Intacs, intracorneal rings, are sometimes used to improve contact lens fit.
Call 281-407-9062 for an appointment.
Riboflavin Corneal Collagen Crosslinking
Corneal crosslinking is a new treatment option under investigation, to halt the progression of keratoconus. In severe cases, a corneal transplant may be needed due to scarring, extreme thinning or contact lens intolerance. This is a surgical procedure that replaces the keratoconus cornea with healthy donor tissue. CXL works by increasing collagen crosslinks, which are the natural “anchors” within the cornea. These anchors are responsible for preventing the cornea from bulging out and becoming steep and irregular.
During the corneal crosslinking treatment, custom-made riboflavin drops saturate the cornea, which is then activated by ultraviolet light. This process has been shown in laboratory and clinical studies to increase the amount of collagen cross-linking in the cornea and strengthen the cornea Collagen crosslinking is not a cure for keratoconus. The aim of this treatment is to arrest progression of keratoconus, and thereby prevent further deterioration in vision and the need for corneal transplantation. Glasses or contact lenses will still be needed following the cross-linking treatment (although a change in the prescription may be required) but it is hoped that it could limit further deterioration of vision.
This procedure, developed at the Technische Universität Dresden, Germany has been shown to slow or arrest the progression of keratoconus in published European studies. CXL is currently in US Food and Drug Administration (FDA) clinical trials.
Corneal Transplants
Although only 15-20% of those with keratoconus ultimately require corneal transplant surgery, for those who do, it is a crucial and sometimes frightening decision. However, it helps to know more about keratoconus and what to expect before, during and after surgery. Those who do are better prepared and feel more in control of their health care.
In keratoconus, a corneal transplant is warranted when the cornea becomes dangerously thin, or when sufficient visual acuity to meet the individual’s needs can no longer be achieved by contact lenses due to steepening of the cornea, scaring, or lens intolerance. Lens intolerance occurs when the steepened, irregular cornea can no longer be fitted with a contact lens, or the patient cannot tolerate the lens
If you suspect you, or a loved one, may have keratoconus, or if you’re experiencing eye pain, bulging, and severe vision problems, it’s time to seek help from Dr. Goosey.
Call 281-407-9062 for an appointment.

Understanding Ectasia
Ectatic corneas are both a contraindication and an occasional consequence for a LASIK patient, who should have never had the surgery to begin with. In a healthy cornea, when you do LASIK, the cornea maintains its shape, and you receive the benefits from LASIK for a long period of time. But, in an unhealthy cornea, the tissue keeps thinning on its own after the procedure, and you eventually lose the benefits from LASIK. These patients have to go into hard contact lenses to achieve best possible vision. That is why Dr. Goosey is very selective on who he will perform surgery on. Because it can be easy to miss subclinical signs of keratoconus, we use the best corneal topographer available today, the Oculus Pentacam. It can detect even the most negligible signs of ectasia or keratoconus.

Unstable Radial Keratotomy
Radial Keratotomy (RK) was a refractive procedure for treating myopia, (nearsightedness) that was very popular throughout the 80’s & 90’s. A flattening of the cornea was achieved by making radial incisions in the cornea. The number of incisions in the cornea, were commensurate with your degree of myopia. Some patients had as many as 16, or even up to 64 incisions in their cornea. The problem with RK is that it was a very unstable procedure. Over a period of 15 to 20 years of the cornea flexing due to changes in intraocular pressure, the cornea collapses centrally and the patient is left with hyperopia (farsighted). But, there is good news for post RK patients, we are able to enhance these patients with either LASIK, PRK, or a Lens Exchange procedure with a monofocal intraocular lens. Multifocal Intraocular Lenses are a contraindication for post RK patients, because the optics in the lens will cause severe glare and halos for these patients.


