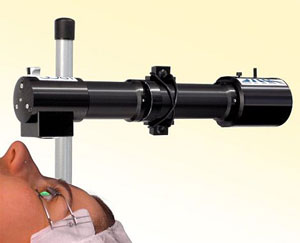
The cornea specialist cross-linking technique is simple and it involves the topical application of a riboflavin solution to the cornea. The superficial epithelial covering of the cornea is removed and the riboflavin drops are then dripped on to the eye.
Corneal Cross-Linking: The Actual Technique
The solution is then activated by application of a UV-A lamp for 20 to 30 minutes or more. According to cornea specialist researchers, the UV excitation converts the riboflavin into excited singlet and triplet states. These excited states then work on the collage fibrils in two different ways. In one process (T1), the oxygen level during the procedure is regulated to a low amount causing the formation of free radicals or free ions.
In the second process of corneal cross-linking (T2), the excited riboflavin combines with oxygen to create singlet molecular oxygen. Both corneal cross-linking procedures work together to start and continue the collage cross links in the cornea. For example, in the first 15 seconds after the eyeball is exposed to the UVA rays, oxygen is still available for the riboflavin and the T2 process starts immediately. During these few seconds, the oxygen, riboflavin and UV light work together to cause a sensitized photo-oxidation of the proteoglycans in the collage stroma. The cornea specialist process occurs to the presence of oxygen species only if oxygen is available. As the available oxygen decreases, the T1 process starts. In the T1 process, the UV light and riboflavin start working on the collage fibrils. Covalent cross-linking of the fibrils along with the corneal stroma, proteoglycans, DNA and RNA takes place improving the strength of the cornea. Researchers reinforce the point that the cornea should be exposed only to 20-30 minutes of UV light to prevent permanent damage to the corneal cells resulting in apoptosis and cell death.
Dr. John Goosey is a world renowned corneal surgeon in Houston, TX who knows that the advantage of corneal cross-linking with riboflavin is that it not only improves corneal health but at the same time, absorbs extra UV light and limits the corneal damage that may occur during treatment. At present, researchers of corneal cross-linking are not really sure how the cross links start and continue. However, carbonyl and free amine groups are commonly seen in the cornea after treatment and carbonyl-based cross-links are predominant. Cornea specialist studies have also shown that the treatment could not only strengthen collagen fibrils but it could also improve linking with other proteoglycan core proteins like mimecan and decorin.
Corneal Cross-Linking: Effects Immediately After Ophthalmology Treatment
• CXL immediately increases corneal rigidity right after treatment but the thickening is limited to the upper 200 ?m of the cornea.
• Ophthalmology studies also show an approximate 12% increase in the constituent collagen fibrils and their strength immediately after treatment.
• Ophthalmology side effects like corneal edema, stromal scars, infections, etc have been reported after the procedure but additional research is required.
Ophthalmology Corneal Cross-Linking: The Best Strategy for Progressive Keratoconus in Ophthalmology
At present, corneal cross-linking is the best option for patients with keratoconus in ophthalmology simply because it is simple and effective. Almost every ophthalmology keratoconus patient can have the procedure done and the ophthalmologic disease can be delayed for as long as 10 years. However, FDA approval has not come through at the time of writing.
Dr. Goosey is the Specialist’s “Specialist” – a corneal specialist, American Board of Ophthalmology board certified and the doctor of choice for many ophthalmologists and other surgeons to perform eye surgeries for themselves as well as their families.